April 16, 2025
The Unit Cost Programme team from the University of Kent and University of York would like to invite you to a series of lunchtime webinars for you to find out more about the Unit Cost Programme.
Why would this webinar be of interest to me?
- Would you like to find out about what Unit Costs are, how they are used and how they could be of interest to health and social care colleagues and members of the public?
- Do you use the annual Unit Cost Manual and would like to find out more about how this is developed?
- Would you like to find out about our new Unit Cost adjuster, which allows you to calculate Unit Costs in a more accessible and interactive way?
- Would you like to input into discussions about the research?
If so, please come along to our webinars to find out more and to ask questions to our team!
When are the webinars and what will they cover?
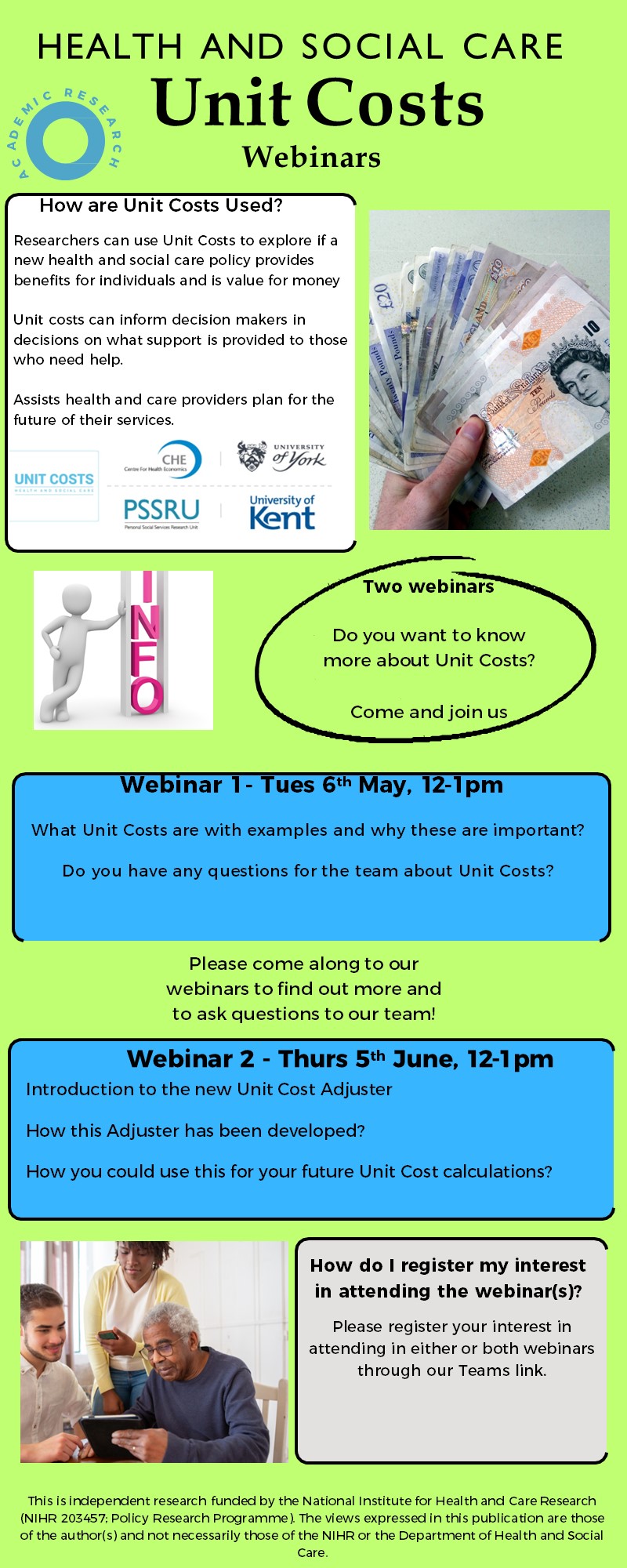
We currently have 2 online webinars planned for 2025:
Webinar 1 – ‘An Overview of the Unit Costs Programme’ (Tuesday 6th May, 12-1pm): In this webinar various members of our team will discuss what Unit Costs are, with examples, and why these are important. This will be of interest to people who use the Unit Costs Manual, people who are new to the Unit Costs Manual, health and social care colleagues and members of the public. You will have the opportunity to ask any questions you have about the Unit Costs Programme during our dedicated Q+A session!
Webinar 1 – Teams Registration Link
Webinar 2 – ‘An Introduction to the new Unit Cost Adjuster’ (Thursday 5th June, 12-1pm): In this webinar, we will introduce the new Unit Cost Adjuster with a demonstration, and provide an overview of how this has been developed and how you could use this for your future Unit cost calculations in a more accessible and interactive way. This will be of interest to people who want to find out more about this new tool for cost calculations.
Webinar 2 – Teams Registration Link
How do I register my interest in attending the webinar(s)?
Please register your interest in attending in either or both webinars through our Teams registration links. If you have any questions or accessibility needs, please contact our Public Involvement and Engagement manager, Sarah Birch (email: s.j.birch@kent.ac.uk; 01227 824967). Please note, we will not be able to cover any public involvement time or expenses for attending this webinar series.