June 9, 2020
 By Dr Stephen Allan, Research Fellow at PSSRU
By Dr Stephen Allan, Research Fellow at PSSRU
Many of us will have relatives and friends that live or work in a care home and so we will have some idea of what is going on within them during the pandemic through both this and the increasing press coverage. As we hear the news of the increasing number of deaths in care homes, two important questions to address are how likely a particular care home is to be impacted by the pandemic and to what extent. Here I briefly present some of the background and then discuss what could influence which homes are more likely to be significantly affected by the pandemic.
Have you seen a care home?
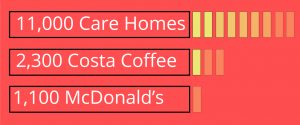
There are over 11,000 care homes registered with the Care Quality Commission (CQC) to provide support to the elderly and those living with dementia in England. To put that in to some context: there are around 1,100 McDonalds and 2,300 Costa Coffee shops. Care homes are an often hidden-in-plain-sight part of a large number of local communities. Care homes for the elderly vary in size from the very small, specialist home to the very large nursing home, and the average size of a care home in England is almost 40 beds. With around nine out of ten beds in care homes occupied on average, this means that there are around 400,000 older residents of care homes in England.
COVID-19 is disproportionately leading to increased hospitalisation and deaths of the elderly. Given the total number of elderly care home residents in England is bigger than the population of Leicester, Nottingham, Newcastle-upon-Tyne, or Brighton and Hove, it is extremely important for appropriate public bodies to consider the impact COVID-19 could have, and is already having, on care homes.
COVID-19 in care homes
There is a lot of research into the spread of infectious diseases in care homes. These are ideal environments for the spread of disease and, unfortunately, this includes the spread of COVID-19. COVID-19 is transmitted through respiratory droplets, either directly or from hands and surfaces. In a care home, there can be a lot of communality between the residents, sitting and dining rooms for example, which makes prevention of transmission between individuals more difficult. Further, residents will require personal and nursing care which means frequent interactions with staff.
All care homes and their staff are naturally trying their very best to support their residents in extremely difficult circumstances. Most if not all care homes are now closed off from visitors. Staff will be well trained and careful with infection control, and additionally in these trying times they are also learning new skills. Some care homes even have staff that have moved in to reduce the threat posed by COVID-19.
What factors will affect whether a home is likely to be affected by COVID-19?
Nonetheless, certain characteristics of a care home and its residents could impact on the likelihood of: a) one resident contracting the infection and b) the spread of infection between care home residents. For example, a bigger care home may increase interactions between staff and residents alike. Additionally, the characteristics of residents will impact on how easy it is to prevent transmission within a home. Those with high nursing care needs will be in contact more frequently with a greater number of staff and those living with dementia are less likely to be able to follow prevention methods such as hand hygiene. Put this way, all three of these home and resident characteristics may increase the likelihood of one resident infection in a care home and potentially the size of the outbreak.
Other factors
However, it is equally feasible to consider alternatives to these arguments. For example on the size of a home, smaller homes with little space will have more close interactions between residents and staff and reduced opportunity to separate residents. In nursing homes, those with very high needs may be confined to their beds and so will have fewer interactions with other residents. Another example is that we might expect homes we consider as higher quality to be more open to their community (engagement events and performers, for example), which may have increased the likelihood of infection, particularly before lockdown conditions.
Additionally, and perhaps crucially, other factors are likely to play a role in the likelihood of infection in a care home, many beyond their control. Local rates of infection, the differing response of respective local authorities to the pandemic and the availability of Personal Protective Equipment (PPE) are all very important factors that will probably impact on the spread of COVID-19 into and within care homes.
What about care home quality?
Could the quality of a care home also play a role in the likelihood of COVID-19 infection? The CQC gives ratings from inspections of care homes. These ratings of a care home (either inadequate, requires improvement, good or outstanding) are based on the answers to five key questions asking if the care home is: safe, well-led, caring, effective and responsive. We might reasonably hypothesise for given levels of resident and home characteristics that one home rated more poorly than another for some of these questions may be more likely to have a COVID-19 outbreak. For example, a home that has a lower well-led rating may have more agency staff working for them and a home with a lower safety rating may have poorer quality infection control protocols in place.
As part of the ongoing NIHR-funded Measuring and Improving Care Home Quality (MiCareHQ) project we are assessing how staffing factors such as wages and job vacancies affect the quality of a care home using a national staffing database (Skills for Care’s Adult Social Care Workforce Data Set). We measure quality using CQC ratings and in the analysis we control for size of home, type of home (nursing vs residential), type of resident (home registered to support those living with dementia) and additionally the sector of the home (private vs voluntary). We can therefore explore how these care home and resident characteristics affect quality ratings.
Findings
We find in our analysis of over 11,000 care home observations over three years that the voluntary sector has a greater likelihood of higher quality for three of these key questions (Safe, Well-led and Responsive) and the overall quality rating, a finding that is in line with our past research. If quality is important then we might expect voluntary sector care homes less likely to be impacted by COVID-19.
Additionally in our analysis we find that nursing homes, larger homes and homes registered to support those living with dementia, all characteristics argued above to potentially increase the likelihood of infection, are all much more likely to have lower quality ratings for the five key questions. As such, CQC quality ratings may be a way to indicate the likelihood of infection.
Overall
Ultimately, each care home is unique and their quality varies from one home to the next – there are some highly rated nursing homes for example. What we can take away from this discussion is that factors outside of a care home’s control and both resident and home characteristics could play an important part in the likelihood of a care home having an outbreak of COVID-19 and the size of the outbreak. Given these factors, the quality of a care home may then also impact on the likelihood of resident infection. Finally, CQC’s quality ratings may be a practical indicator of the likelihood of a care home suffering an outbreak given that many of the care home and resident characteristics we think could potentially impact on infection likelihood are also found to affect quality ratings negatively.
The data relating to COVID-19 is not yet available at individual care home level to allow us to explore these issues in more detail. This research will no doubt look to understand why certain care homes had outbreaks, to what extent, and what can be done to mitigate infection within care homes in the future, and these will be some of the main factors analysed.
Time of concern
We are all having to deal with changes to our daily lives during this pandemic, but for care homes the threat of this pandemic is apparent and very real. Whether or not you know someone living or working in a care home, if you walk, run or cycle past one on your daily exercise or on your way to work in the coming days and weeks, spare a thought for all those inside at this very worrying time for us all.
Disclaimer
The MiCareHQ project is funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (reference 15/144/51). The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care.